
Although the European epilepsy day has been over for a few days, it’s still important to understand this neurological disease. Therefore, this blog post discusses the defintion of epilepsy, the development, consequences and causes of various forms of epileptic seizures and the first advances in personalized treatment.
Definition
Epilepsy is a neurological disorder associated with a malfunction of the brain.1 It’s not a single disease but rather the result of a multidue of diseases sharing a common tendency to epileptic seizures.2,3 In such seizures the communication between the nerve cells is disturbed leading to a temporary, synchronous discharge of larger nerve cells.4 The diagnosis epilepsy is made when such seizures occur multiple times without apparent triggers.1
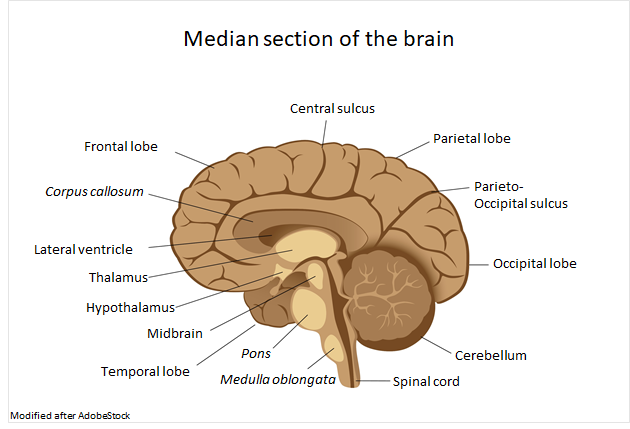
Nerve cells

Nerve cells (neurons) are part of the nervous system. Depending on the localization in the body a distinction between the central nervous system including the neural pathways in the brain and spinal cord, and the peripheral nervous system is made.5 The human body contains several billions of neurons, only our brain contains 100 billion nerve cells.5,6 These are interconnected by electrical and chemical signals.6 Nerve cells consists of a body and several appendages.5 The dendrites act as antennas, through which the body receives the signals.5 Via the longer extension, the axon, the signals are transmitted.5
Formation and consequences
When an epileptic seizure is happen, this interaction is temporarily disturbed and the brain is excessively active.6 Neurons of the cerebal cortex suddenly send signals simultaneously and highly synchronously, forcing their own rhythm to other cells.2 Thus, parts of the brain are overly active for a time, depending on the nature of the seizure.1 This is followed by the post-phase, in which the cells are no longer pathological unloading themselves, but still show abnormalities.1
The consequences are different, depending on
- Where the nerve cells are lying in the brain2
- How many nerve cells are involved2
- Which body functions they control2
A single seizure isn’t dangerous.2 However, in some rare cases a cardiovascular failure called SUDEP (sudden death of epilepsy patients) can occure.2
Causes
The cause of a seizure is sometimes directly attributable to a specific trigger, for example genetic changes, a stroke or a brain tumor.2 Often, however, the exact development of the disease is obscure.1
- Cryptogenic epilepsy: no specific cause can be found, although there’s evidence in the brain.1
- Idiopathic epilepsy: there’s no evidence of a cause or pathological change in the brain.1

- Genetic epilepsy: genetic alterations for example at binding sites (receptors) for neurotransmitters1
- Symptomatic/structural/metabolic epilepsy: structural changes in the brain, for example congenital malformations, brain damage acquired at birth, stroke, inflammation or metabolic disorders (Diabetes).1
Classification
Epileptic seizures may vary in severity.2 From a few seconds of mild muscle twitching to several minutes of spasms and loss of consciousness.2 In general, seizures can be grouped into three categories:
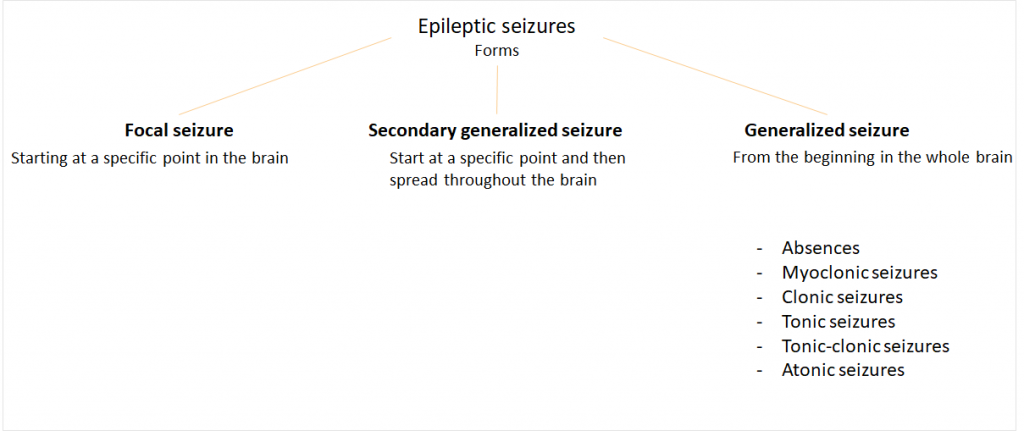
Focal seizures always start at a specific point in the brain, for example at an injury.7 Most of them beginn with a so-called aura, in which unusual sensory impressions such as visual disturbances, concentration disorders or dizziness are recorded.7 The complex-focal form is also associated with a loss of consciousness.7
Generalized seizures spread from the beginning throughout the brain, leading to temporary disturbances of consciousness.7 Here, the cause can rarely be found.
- People suffering from absences lose consciousness for a few seconds. These occur mainly in children and adolescents.7
- A myoclonic seizure is always associated with twitching of certain muscle groups, for example the hand, arm or the trunk. The consciousness is maintained.7
- Clonic seizures last up to several minutes, in which the muscle groups on the trunk contract rhythmically.7
- In tonic seizures, the muscles cramp together without twitching, the affected often lose consciousness. The duration is only a few seconds.7
- The tonic-clonic seizure also called grand mal starts with an aura, followed by a loss of consciousness. Camps take place all over the body, as well as rhythmic twitches on arms, legs and head. Foamy saliva can come out of the mouth. The skin turns blue as a sign of hypoxia.7
- In atonic seizures, muscle tension in parts of the muscles decreases.7
Epidemiology
There are between 500,000 and 600,000 people confronted with epilepsy in Germany. This corresponds to 0.6% of the population.3,8 Wordwide there are almost 50 million epileptics.9 Industrialized countries, such as Germany, register between 40 and 70 new cases per 100,000 inhabitants annually.1,3
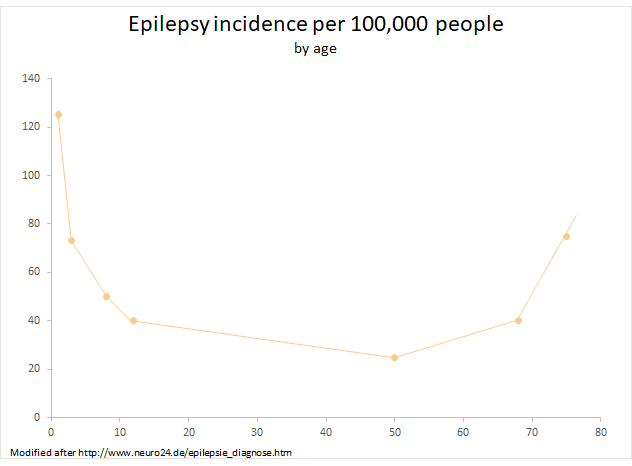
The neurological disease can occur at any age,2 but the risk is particularly high in the first five years of life, accounting for two-thirds of all epilepsy cases.3 For children, it’s the most common disease of the central nervous system.1 From the age of 20 the risk decreases while it rises again at the age of 60.3,10 Age epilepsy is the third morst common brain disease among older people.10
Liftetime risk is understood as the probability of come down with certain disorders in the course of life. In the case of epilepsy this is 3%, in the case of an epileptic seizure 10% up to the age of 80.2 Experts estimate that 5-10% of all people experience an epileptic seizure at least once in their lives.3,6
This risk is also increased among people with certain previous illnesses. 15% of all patients suffering a stroke have epileptic seizures, 10% of them develop epilepsy.3
Treatment
Patients whose epilepsy is genetically determined have the same life expectancy as healthy people.6 The seizures don’t damage the brain, but other illnesses, such as depressions can be favored.6 The so-called status epilepticus isn’t common, but life-threatening.2 This causes seizures of long duration in which the brain can be damaged.2
There is the option of a surgery for patients suffering from focal seizures.1 In the so-called epilepsy surgery parts of the brain are removed, especially if the origin lies in the temporal lobe.1
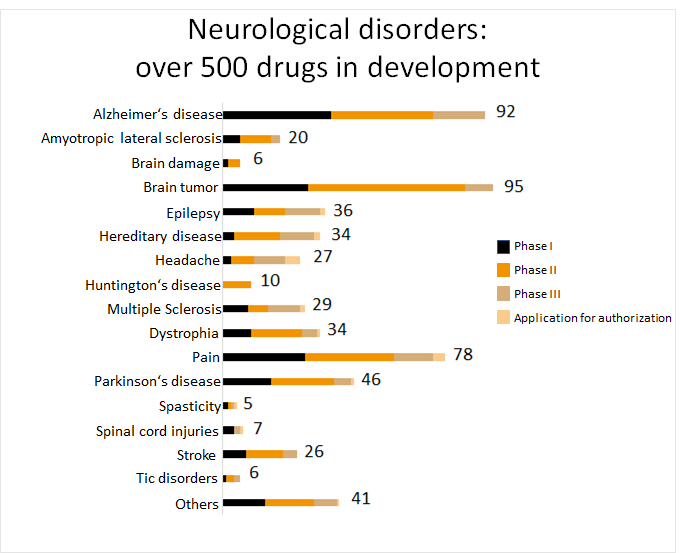
Anticonvulsants inhibit the excessive activity of nerve cells and reduce the risk of suffering from a seizure.1 However, they have only a symptomatic effect and can’t cure the disease.1 There’re currently almost 20 antiepileptic drugs on the market9, with another 36 drugs under development.11
Another problem with anticonvulsants is that only two-thirds of all patients feel a positive effect of the prescribed medication and they can live without further seizures.8 3 out of 10 patients still suffer from epileptic seizures or experience side effects.6,8 In such cases, a genetic analysis can help to predict the efficacy of drugs.8
Progress
Personalized medicine
It has been shown that patients with particular hereditary disposition of the immune system have an increased risk of severe and rare skin reactions after taking oxacarbazepine or carbamazepine.12 This is a matter of a gene of the HLA system.13 Carrier of this gene variant are mainly Han Chinese, Thai, Japanese and other asian populations, but also 5% of the europeans.12 Since 2014 or rather 2013 a genetic test for prescribing the antiepileptic drug is recommended to exclude these side effects.13
New found epilepsy genes
The International League against Epilepsy (ILAE) perfomed an analysis of genetic data from more than 15,000 epileptics and nearly 30,000 unaffected people.14 This allowed them to discover 21 risk genes with different functions involved in the development of the neurological disease.14 One of the functions is the association with ion channels, which transmit the signals in the nervous system.14 Mutations limit the functionality of proteins, which is the basis of epilepsy.14
These findings can be used to personalize the medicine to get therapies more targeted.
Contact person:
Kristina Schraml (kristina.schraml@biovariance.com)




