The Problem
Regular clinical tests demonstrate a serious and growing threat today: resistant bacteria showing immunity against many common antibiotics. The evolution and widespread distribution of antibiotic resistanct pathogens has made diseases that were once easily treatable deadly again. And thus, bear a big challenge in health care for physicians, researchers, politicians and the public in large. [1]
Millions of bacteria can be found in the human body naturally and support the immune system. In contrast, pathogens can cause damage to the body and induce severe symptoms, especially when the number of available antibiotics is low. Drug resistance develops when mutations occur during the multiplication of bacteria. This resistance is inherited to the daughter cells and soon there will exist only resistant variants. Basically, these organisms are not more dangerous than other bacteria, but in the case of an infection it is far more difficult to treat.
An inappropriate application of antibiotics promotes the development of multiresistant bacteria. This includes low dosage, excessive use and shortened application time. [1,2]
Current situation
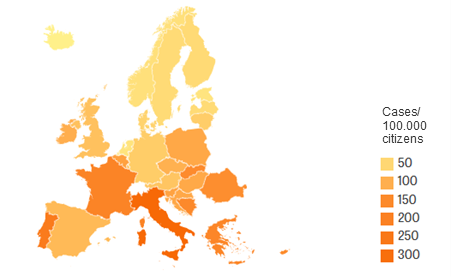
In 2015, nearly 700.000 people got an infection with multiresistant bacteria, while about 33.000 patients died as a result (Fig. 1). Italy had the highest number of new cases (200.000), followed by France with about 125.000 new cases. In Skandinavia, Estonia and the Netherlands, the number was relatively low. In Germany, 55.000 patients caught an infect with resistant organisms. Generally, children younger than 1 year had the highest risk of infection. [2]
About 700.000 patients died of the infection worldwide. [3]
The most feared pathogens
In 2017, the World Health Organization (WHO) published a priority list of antibiotic-resistant bacteria to support research and development of effective drugs. Important criteria were e.g. mortality, healthcare burden, predicted trend of resistance and preventability in hospital and community settings.[4] Bacteria resistant to carbapeneme antibiotics are on top of this list, because these drugs are actually applied in the case of other antibiotic resistances. When carbapeneme cannot be applied, the chance for a successful antimicrobial therapy strongly decreases. [1] Acinetobacter baumannii, Pseudomonas aeruginosa and some Enterobacteriaceae (e.g. Escherichia coli) show carbapeneme resistance and can cause severe lung inflammation, infections and sepsis when the patient has a weakened immune system. Other listed and well-known microorganisms are e.g. Staphylcoccus aureus (MRSA), Helicobacter pylori und Streptococcus pneumoniae. [4]
Progress through Research
New therapeutic options for the treatment and prevention of infections caused by multiresistant bacteria are urgently needed. For this purpose, the EU-project COMBACTE-MAGNET was started in 2015 with a budget of 170 Mio. €. Aim of the project is the development of new antimicrobial treatments for vulnerable patients, especially the critically ill in intensive care units, and the identification of effective biomarkers based on scientific collaborations. More than 30 leading academic medical centres from 10 European countries and experts from AstraZeneca, AiCuris, GSK, Basilea Pharmaceutica, and Sanofi are participating in this project, which is coordinated by Sweden. [5]
Future aspects
Resistant organisms pose a threat to survival rates from serious infections and limit the potential health benefits from surgeries, transplants, and cancer treatment. The challenge of ensuring appropriate access to antibiotics, while restricting inappropriate access, is unique in global health and requires new approaches regarding financing, health care and research. [6] New commercial models must be implemented to make the industry invest in antibiotics development and to ensure simultaneously that new antibiotics are used sustainably. [3]
Contact person:




